Family Devastated as Doctor Euthanizes Diabetic and Blind Man in Canada
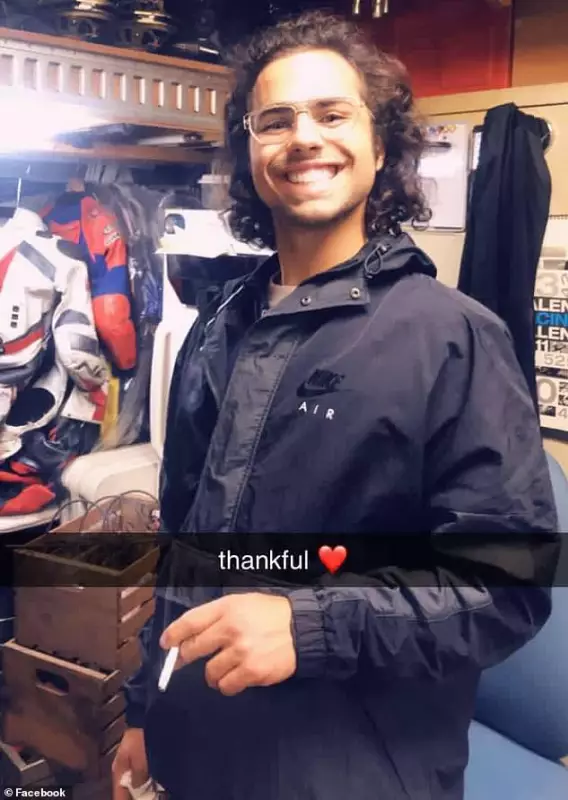
A Canadian family has been plunged into profound grief and anger following the physician-assisted death of their 26-year-old son, who was living with blindness and type 1 diabetes. The tragic incident occurred three years after the family had successfully intervened to prevent him from accessing Canada's Medical Assistance in Dying (MAiD) program.
Mother's Intervention and Subsequent Loss
In 2022, Margaret Marsilla, the young man's mother, managed to stop her son, Kiano Vafaeian, from undergoing euthanasia. Marsilla has consistently argued that her son was not terminally ill, highlighting that his conditions included blindness, complications from type 1 diabetes, and mental health challenges. Despite her efforts, Vafaeian was approved for physician-assisted suicide on December 30, 2025, under Canadian law, which permits such procedures if applicants demonstrate an "intolerable" condition that cannot be relieved under conditions they find acceptable.
Emotional Outcry and Legal Context
Following her son's death, Marsilla expressed her anguish on social media, recalling how they had previously halted his euthanasia in Ontario and secured help for him. She emphasized that he survived because people intervened during his vulnerable state, when he was not capable of making a final, irreversible decision. Marsilla condemned the physician-assisted death as "disgusting on every level" and vowed to fight for her son and other parents with children suffering from mental illness. She lamented that no parent should have to bury their child because a system and a doctor opted for death over care, help, or love.
Expansion of Assisted Dying in Canada
Canada legalized assisted dying in 2016, initially restricting it to terminally ill adults whose deaths were reasonably foreseeable. However, eligibility was broadened in 2021 to include individuals with chronic illnesses, disabilities, and certain mental health conditions. This expansion has sparked ongoing debates about the ethical implications and safeguards within the MAiD program.