Nigeria's fight against HIV/AIDS has reached a critical juncture. The battle has evolved from confronting deep-seated stigma to now fighting for the very continuity of lifesaving antiretroviral therapy (ART). While treatment has transformed HIV into a manageable condition, recent drug supply disruptions, funding uncertainties, and an overreliance on foreign aid have exposed dangerous cracks in the national response. Experts warn that without urgent local investment and resilient health systems, hard-won gains could unravel, putting millions at risk.
From Stigma to Survival: The New Fear of Treatment Disruption
For individuals like Nwanma Aladoh (not real name), the initial shock of an HIV diagnosis was compounded by profound betrayal and social ostracization. "It felt like betrayal from the deepest place," she recounted, describing how her late husband concealed his status. The stigma followed her relentlessly, altering relationships and even manifesting in subtle discrimination within healthcare settings.
However, a newer, more existential fear has now emerged for the estimated 1.9 million Nigerians living with HIV. Grace Omodunbi, who has lived with the virus for 27 years, thought stigma was the ultimate challenge. Recent service disruptions, including temporary lab closures and drug rationing, changed that. "I thought stigma was the hardest part, but now I know that even after overcoming it, our treatment can be taken from us," she lamented.
This anxiety is widespread. Eghosa Obasohan, diagnosed in 1994, recalls when HIV was a death sentence due to inaccessible treatment. While subsidized ART later gave him a lifeline, the recent instability rekindles old fears. "Drugs are available now, yes, but for how long?" he asked. "I'm worried about losing the treatment that has kept me safe for three decades."
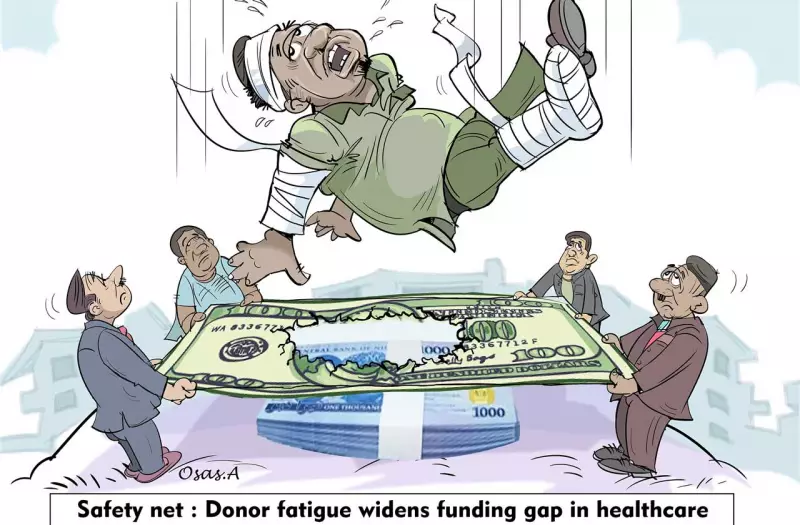
Funding Fragility and the Threat of External Withdrawal
The core of this instability is financial. Nigeria's HIV response remains heavily dependent on international donors. The President's Emergency Plan for AIDS Relief (PEPFAR) covers a significant portion, but its pause in early 2025 under the U.S. Trump administration sent immediate shockwaves through the system. Although a waiver later restored medicine supplies, the episode highlighted a dangerous vulnerability.
Compounding this is the proposed "sunset" of UNAIDS by the end of 2026 as part of UN restructuring. This has sparked alarm among civil society and health advocates who fear the dissolution of the world's only dedicated HIV agency could reverse global progress. For Nigeria, which also relies on UNAIDS for funding and coordination, the implications are stark.
Mr Abdulkadiri Ibrahim, President of the Network of People Living with HIV/AIDS in Nigeria (NEPWHAN), acknowledges progress but underscores the uncertainty. "Even though the treatment is available, the uncertainty is still there because we don't know what will happen in the next couple of years," he stated. He pointed to the $200 million approved by the Federal Government for HIV, TB, and Malaria as a positive step, but stressed that sustainability requires consistent government ownership and investment.
Uneven Progress and Vulnerable Populations
National data shows a mixed picture. The National Agency for the Control of AIDS (NACA) reports that Nigeria is close to the global 95-95-95 targets: 87% of people living with HIV know their status, 98% of those diagnosed are on treatment, and 95% on treatment are virally suppressed. However, prevalence remains alarmingly high in some regions, like the South-South zone at 3.1%, with Akwa Ibom (5.5%) and Benue (5.3%) bearing the heaviest burden.
Critical gaps persist among key populations. A field study by the Nigerian Institute of Medical Research (NIMR) found an astonishing 12% HIV prevalence among previously unscreened adolescents and young adults—nearly ten times the national average. Furthermore, key groups like sex workers, men who have sex with men, transgender women, and people who inject drugs continue to bear a disproportionate burden of new infections.
Prof. Alani Akanmu, former Chairman of Nigeria's National ART Task Team, emphasized the strategic importance of serving these populations. "This population... is contributing more than 20% of new infections in the country. And if truly we think we want to end the HIV epidemic, then we cannot neglect to deliver to them all HIV programme services," he argued.
Another persistent challenge is the prevention of mother-to-child transmission (PMTCT). Esther Hindi, National Coordinator of the Association of Women Living with HIV/AIDS, noted that stigma still drives pregnant women away from treatment, leading to preventable paediatric infections. "The key driver is stigmatisation and discrimination. We want an end to paediatric HIV in Nigeria," she said.
The Urgent Call for Local Ownership and Sustainable Solutions
Faced with these intersecting challenges, stakeholders are issuing a unified call for change. The Association of Community Pharmacists of Nigeria (ACPN) has urged urgent local investment in manufacturing antiretrovirals and diagnostics to reduce external dependency. Publicity Secretary of NEPWHAN Lagos, Ahmed Salisu, warned that many patients cannot afford to pay for medications if free supplies stop, making government ownership of treatment provision non-negotiable.
Kayode Emmanuel of the Reach Care Foundation Nigeria offered a sobering perspective: Nigeria's gains cannot withstand further shocks. He explained that any cut to programmes like PEPFAR threatens stockouts, reduced testing, and loss of patient follow-up, which can quickly reverse progress and fuel new infections.
The message is clear. As the 2025 World AIDS Day theme, "Overcoming Disruption, Transforming the AIDS Response," urges, Nigeria must prioritize innovation and community empowerment. The progress that turned HIV from a death sentence into a manageable condition is real but remains perilously fragile. The path forward demands strong local investment, sustainable funding, and a health system resilient enough to protect millions of lives from the threat of a preventable setback.